Tracking Reactive Species Opens Path to Plasma Diagnosis
हिंदी में सुनें
Listen to this article in Hindi
Real-time monitoring of reactive oxygen and nitrogen species (RONS) during cold atmospheric plasma treatments improves dose control and therapeutic effectiveness.
Cold atmospheric plasma is finding increased use in medical applications like wound treatment, decontamination, and cancer therapy. The beneficial effects largely stem from reactive oxygen and nitrogen species (RONS), such as hydrogen peroxide (H2O2), which are important for controlling inflammation, fighting microbes, and repairing tissues.
That said, the reality is a bit more complicated. controlling the dosage remains a significant hurdle. Insufficient plasma may not be effective, while excessive amounts can lead to oxidative damage and hinder the healing process.
Traditional methods for plasma diagnostics, like monitoring electrical signals or using optical emission spectroscopy, are useful in industrial settings. That said, the reality is a bit more complicated. they don't provide enough information about biological outcomes and aren't practical for clinical use.
The researchers in this study propose that monitoring the chemical species that directly interact with tissue, in real time at the treatment site, is the most relevant way to control plasma dosage from a clinical perspective.
**Sensors Inside the Treatment Zone**
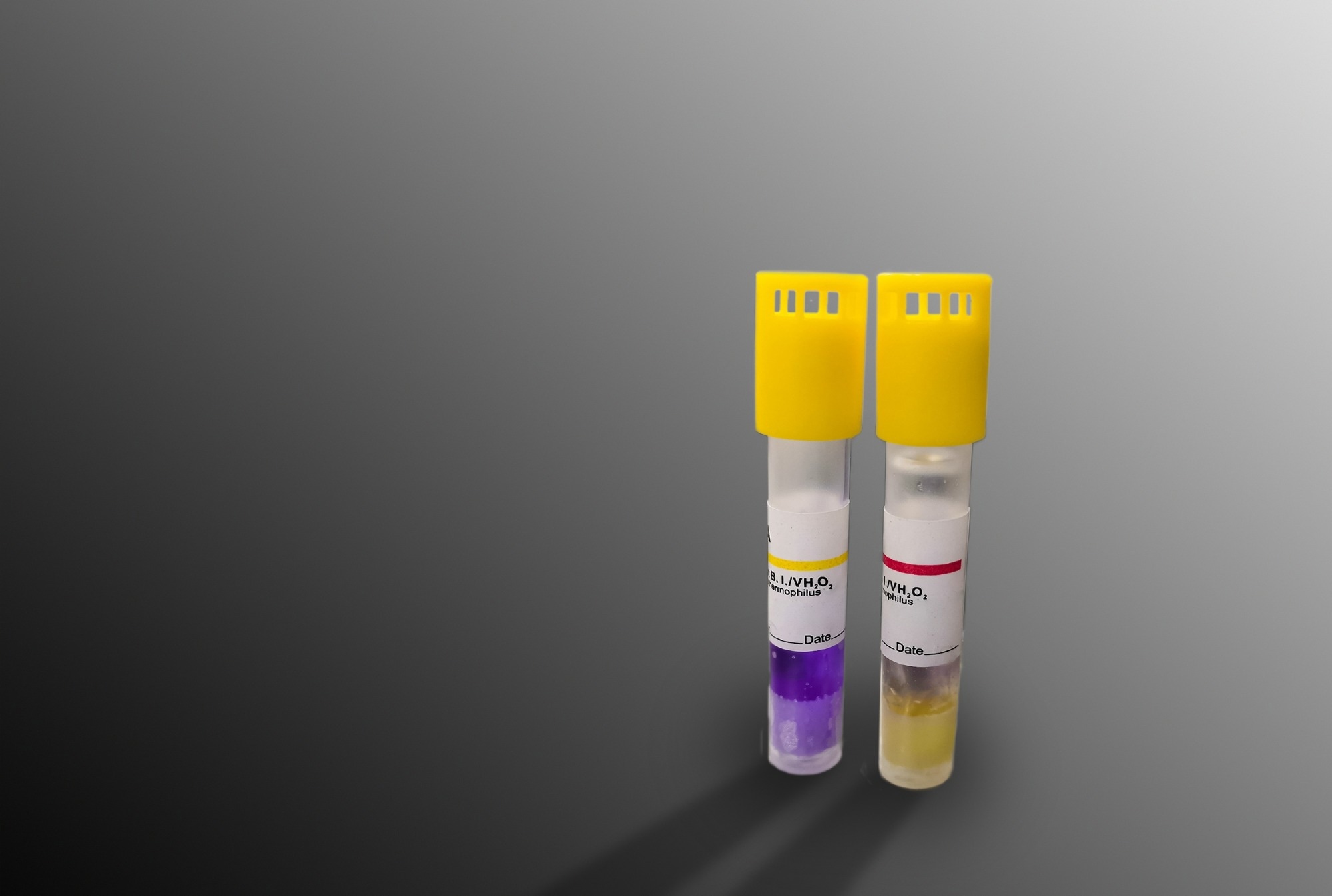
To achieve this, the team employed commercially available, non-enzymatic wire sensors. These sensors are small enough to function directly within liquids, cell cultures, and even living tissue.
The sensors measure two complementary indicators: hydrogen peroxide concentration and oxidation-reduction potential (ORP). ORP is a voltage-based measurement reflecting the overall redox state created by multiple oxidants and antioxidants.
Both sensor types use a platinum-iridium working electrode, designed to withstand exposure to highly reactive plasma species. The hydrogen peroxide sensor incorporates a Nafion membrane to improve selectivity, while the ORP sensor remains uncoated to measure the overall oxidative environment.
Sensor signals were processed using either commercial potentiostats or a custom microcontroller, enabling the system to be integrated into a compact, portable unit.
**Linking Chemistry to Biology**
By using *in vitro* scratch assays and *in vivo* mouse wound models, the scientists correlated real-time sensor readings with biological outcomes. These outcomes, measured hours to weeks later, included wound closure rates, cell proliferation, oxidative stress responses, and scar formation.
The results showed a clear pattern between dosage and response. Moderate plasma exposure accelerated healing and reduced scarring, whereas higher doses increased oxidative stress, leading to temporary delays in recovery.
Rather than pinpointing a single causative molecule, the study highlights the correlations between measured RONS levels and subsequent biological effects. This is a practical approach, considering the complex interactions between plasma and tissue.
ORP measurements proved particularly valuable in capturing the overall redox environment. They complemented hydrogen peroxide readings and demonstrated how different tissues exhibit varying baseline oxidative states.
**Control in Living Tissue**
The most notable advancement was incorporating the sensors into a closed-loop control system. During treatment, hydrogen peroxide levels were continuously monitored using pulsed chronoamperometry, a technique that minimizes signal interference caused by plasma ignition.
Instead of applying plasma for a set period, the system automatically stopped treatment once hydrogen peroxide levels increased by 25 micromolar above the initial baseline. This threshold was intentionally conservative, based on lower-quartile responses observed across animals, to minimize the risk of overexposure.
In live mouse wounds, the controller consistently ended treatment at varying times, depending on baseline conditions, the wound environment, and individual biological differences. This demonstrates dose-based control, as opposed to time-based delivery.
**A Future of Adaptive Plasma Medicine**
While the system isn't yet designed for personalized patient treatment, the study provides a practical framework for adaptive plasma therapies. These therapies can respond to real-time biological conditions. By accounting for baseline variability across different tissues and environments, sensor-driven feedback offers a more dependable alternative to fixed treatment plans.
The authors acknowledge that further work is necessary to address sensor durability, sterilization procedures, and regulatory requirements before clinical use.
That said, the reality is a bit more complicated. the findings suggest that integrating electrochemical sensing into plasma devices could significantly enhance safety, consistency, and therapeutic efficacy.
Although the experiments centered on wound healing, this approach could be applied to other plasma-based treatments, including cancer therapy and infection control. More broadly, the study demonstrates how incorporating real-time chemical sensing into medical devices can bridge the gap between delivering a physical dose and achieving a desired biological response.